Obstructive lung disease (OLD) includes COPD and asthma. By 2020, OLD will be the third leading cause of death.
Asthma
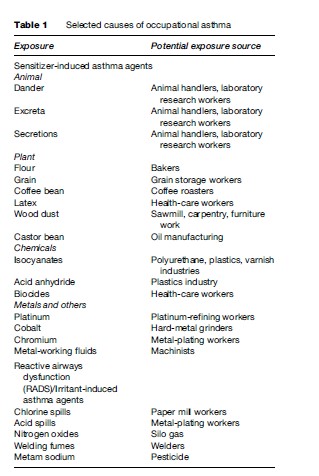
Over 250 substances have been identified as causes of asthma, which is characterized by airway inflammation and is associated with intermittent spasm of the airway smooth muscle. Asthma can be work aggravated, an exacerbation of subclinical disease, or new onset. Sensitizer-induced asthma develops a few months after exposure because it takes the body that long to develop antibodies to the exposure. Sensitizers include high and low-molecular-weight chemicals. High-molecular-weight chemicals stimulate the production of IgE, an allergic antibody, and include biological proteins such as particles from wood products, textiles, grains, crustaceans, and latex allergen. Low-molecular weight chemicals, such as isocyanates (chemicals used in polyurethane foams and paints), react and combine with endogenous chemicals already found in the body to produce allergens which in turn stimulate the production of antibodies. Nonspecific irritants can provoke work-aggravated asthma.
Respiratory toxicants can be divided into allergens and irritants. Irritants initiate disease by mechanical, thermal, and chemical irritation of local nerve receptors. Allergens (sensitizers) react with antibodies to trigger an immunological cascade leading to disease. Antibodies are molecules in the blood and secretory fluids of the body that tag, destroy, and neutralize bacteria, viruses, and other toxins. The immunological cascade triggered by these antibodies includes a network of different cells and the chemical products they produce that protect the body from these foreign invaders. Reactive airways dysfunction (RADS), or irritant-induced occupational asthma, may occur after a single, massive irritant exposure or repeated, smaller ones. Unlike sensitizer-induced asthma, RADS occurs immediately after massive exposure because it is caused by irritation and does not involve stimulating the body’s internal immunologic cascade.
Diagnosing occupational asthma requires taking a careful history with specific attention to the relationship between symptoms away and at work. Workers with an individual or family allergy history are at increased risk. Symptoms are often episodic and include coughing, wheezing, chest tightness, and shortness of breath. Breathing studies such as pulmonary function tests performed at and away from work are helpful (Table 1).
In addition to exposure avoidance or reduction through respiratory protection, treatment entails the use of standard asthma medications. This includes inhalers such as inhaled corticosteroids and oral medications such as leukotriene antagonists that reduce inflammation. Other classes of medications also include long-acting beta-agonists, which relieve bronchospasm, or airway muscle spasm. In workers with sensitizer-induced disease, environmental controls and respiratory protection may be insufficient because low exposure levels can trigger symptoms. Early recognition and prevention are crucial because symptoms may persist after exposure discontinuation.
Chronic Obstructive Pulmonary Disease
Unlike the intermittent airflow obstruction found in asthma, COPD is characterized by chronic airflow obstruction. While COPD is predominantly associated with tobacco smoking, workers in coal mines, hard rock mines, tunnel workers, and concrete-manufacturing workers are also at increased risk. Although there are two forms of the disease – emphysema (destruction of the alveoli) and chronic bronchitis (airways clogged with mucus due to chronic inflammation), the most common form is a combination of these two and often also overlaps with asthma. Symptoms of chronic cough and shortness of breath may not present until many years after exposure onset. Diagnostic workup includes breathing studies such as pulmonary function tests. Several medications are available that relieve inflammation (e.g., inhalers that contain steroids) and muscle airway spasm (e.g., anticholinergic and betaagonist inhalers). In general, COPD treatment is not nearly as effective as asthma treatment because the damage in COPD is often irreversible.
Diseases Of The Respiratory Units Or Lung Parenchyma
Several widely prevalent respiratory toxicants cause fibrosis or scarring of the lung parenchyma – the internal tissue in the lung – or pleural disease, which is disease of the lung lining. Most cases are due to asbestos exposure, silica and coal dust exposure from working in coal mines, exposure to beryllium (causing chronic beryllium disease), and organic dust (causing hypersensitivity pneumonitis).
Asbestos Lung And Pleura Effects
Asbestos is a strong incombustible fiber, which is used for fireproofing and insulation and comprises several forms including chrysotile, amosite, crocidolite, and tremolite. Shipyard workers, electricians, welders, and plumbers all may be potentially exposed. Even moderate, cumulative exposure to asbestos over years can result in various pulmonary manifestations involving either the pleura – the lung lining – and/or the lung parenchyma. Disease may be relatively benign, such as in the case of pleural effusions, a fluid collection between the two layers of lung lining, or pleural plaques – scars of the lung lining studded with calcium deposits. Disease of the lung parenchyma including scarring and pulmonary fibrosis may range from mild to severe. Finally, exposure may cause cancer, primarily lung cancer and mesothelioma (a unique form of cancer of the pleura).
Workers with benign disease (e.g., pleural disease) may be asymptomatic, whereas workers with more severe disease (e.g., pulmonary fibrosis) may develop the insidious progression of shortness of breath and nonproductive cough. In the case of the latter, unfortunately, treatment options are limited. Diagnostic evaluation for workers with pulmonary fibrosis may reveal reduced lung volumes – that is, a restrictive ventilatory defect, on lung function tests. Radiographic imaging for workers with pulmonary fibrosis may reveal mild scarring (small, linear, irregular lines) at the lung bases, or bottom of the lungs (Figure 2).