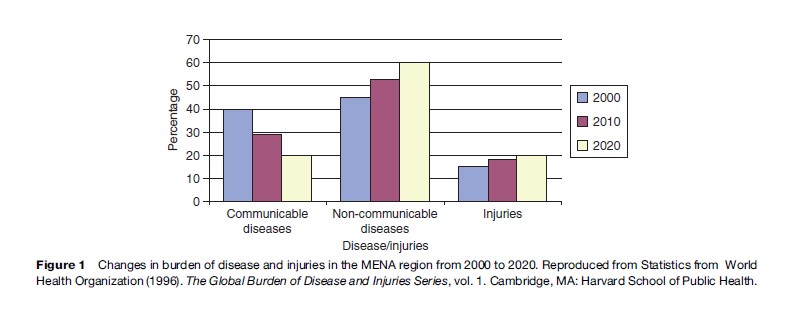
Gaziano (2007) notes that the region as a whole seems to be entering the third stage of the epidemiological transition characterized by degenerative and man-made diseases, although a number of countries are facing a dual burden of disease characterized by decreasing rates of communicable diseases and increasing rates of noncommunicable diseases (NCDs). WHO estimates for MENA indicate that communicable diseases will account for 29% of the disease burden in 2010 (an 11% decrease from 2000) while NCDs will account for 53% (8% increase from 2000) (Figure 1). The same estimates predict that communicable diseases and NCDs will account for 20% and 60%, respectively, by the year 2020. Of particular significance among NCDs in the region is the incidence of cardiovascular disease (CVD) and diabetes. Like other developing regions (with the exception of sub-Saharan Africa), CVD is the leading cause of death in MENA, which, according to Wild et al. (2004) also faces the highest projected increase in the number of cases of diabetes from 2000 to 2030 (164% increase from 20 million in 2000 to 52.8 million by 2030).
For low-income countries and rural areas in middle-income countries like Egypt and Morocco, where communicable diseases are still a significant burden, they are concurrently experiencing an increasing burden of NCDs dispelling previous notions that NCDs mostly affect the affluent populations. Various research results by the Global Burden of Disease project have indicated that premature mortality rates from NCDs are actually, on the one hand, higher in populations with high mortality and low income than in industrialized countries. Middle and upper-income countries in MENA, on the other hand, are mainly burdened by NCDs, having largely eliminated communicable diseases.
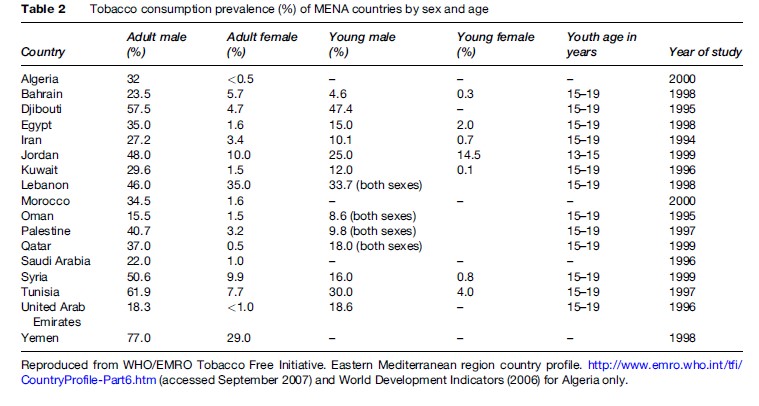
The effects of rapid urbanization (60% of MENA’s population live in urban areas) and changes in diet and lifestyle are significant contributing factors to the rising rates of NCDs in the region. Of public health concern is the increasing prevalence of tobacco use in the region where tobacco-related deaths were projected by Murray and Lopez (1996) to increase from 2.4% in 1990 to 9.5% in 2020. Global smoking prevalence data presented by Jha et al. (2002) reveal that the overall MENA prevalence was 23%, less than the global average of 29%. Data from WHO/EMRO for subsequent years (1996–2000) indicate that the smoking prevalence rates in the MENA region are increasing (Table 2) with prevalence rates among men ranging from 15.5% in Oman to 77% in Yemen.
The region is also experiencing a nutrition transition characterized by a high prevalence of stunting from undernutrition particularly in low-income countries and certain geographic areas of middle to high-income countries. There is also widespread iron-deficiency anemia and other micronutrient deficiencies and newer problems related to obesity from overnutrition and their links with NCDs/chronic conditions. The adoption of Western lifestyles of decreased physical activity and significant increases in the consumption of energy-dense foods have led to significant increases in the prevalence of overweight and obese populations. MENA along with the Pacific Islands, Southeast Asia, and China face the greatest threat of increasing prevalence of overweight and obese children in the world.
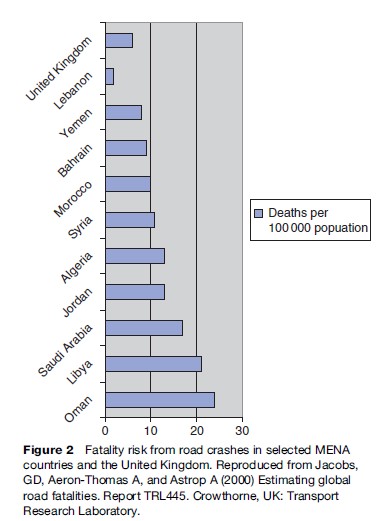
The rising numbers of road traffic accidents (RTAs) is also becoming a major cause of premature mortality in the region. Road traffic injuries are the major cause of injuries in the region, the burden of which is expected to increase from 15% in 2000 to 20% in 2020 (see Figure 1). According to WHO, there was a dramatic increase (20%) in the number of deaths due to RTAs from 1980 to 1995 and the trend has continued since then. Kopits and Cropper (2003) indicate that in 1990 there were about 41 000 road traffic fatalities in MENA and predict that this number will be 94 000 in 2020, a 68% increase. The MENA region also has a greater share of global road crashes than would be expected from the number of vehicles and population of the region. Peden et al. (2004) reported that at 26.4 deaths per 100 000 population, low and middle-income countries of MENA have among the highest rates in the world (compared to a global rate of 19 per 100 000). Figure 2 demonstrates road crashes-related death rates per 100 000 population of selected MENA countries, which are generally higher than the rate for the United Kingdom.
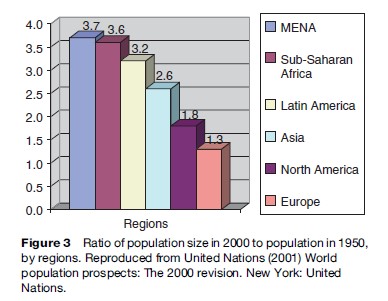
From 1950 to 2000, MENA experienced a 3.7-fold increase in population, the highest population growth rate in the world (Figure 3) and currently has the second highest annual population growth in the world (at 2% or nearly 7 million additional people per year). At this rate, MENA’s population is projected to double in about 50 years (Population Reference Bureau, 2001). As the population rates are increasing in the region, so are the death rates decreasing leading to a rapidly expanding youth population, with 58% of the population less than 25 years old (UN, 2006) and a more modest expansion of the aging population. Countries of the region are however at different stages of the demographic transition, ranging from those in the early transition stage with both high birth and death rates such as Yemen and Djibouti, right up to those considered to have essentially completed the transition with both low birth and death rates such as Bahrain, Kuwait, Qatar, and United Arab Emirates. All the countries, to differing degrees depending on their stage in the transition spectrum, will have to address both a population momentum that could strain existing health systems as well as the specific health needs of an aging population.
Migration to, from, and within the region is also a significant contribution to the population momentum in MENA. Not only has the region had the largest population and labor flows in the past 50 years, but it also has the largest refugee population in the world. The oil-exporting countries of the region have hosted millions of foreign workers since the oil boom of the 1970s, with foreign workers constituting anywhere from 60–90% of workers in these countries. Arabs from other MENA countries and Asians from Pakistan, India, the Philippines, and Indonesia make up the majority of the foreign workers in the oilexporting countries, which also have to provide services to address health concerns of the workers and their families. Countries of the region hosting refugee populations are also challenged to provide them with health services.
Emerging Diseases
Like the rest of the world, newer diseases such as HIV/ AIDS and highly pathogenic avian influenza (HPAI) are emerging in MENA and posing new challenges. While HIV prevalence rates in MENA are still low and largely limited to high-risk groups (who are also highly marginalized and difficult to reach), the risks for further spread exist and unless effective and timely preventive measures are implemented, the disease could have significant social and economic consequences. Jenkins and Robalino (2003) estimate that health-related HIV/AIDS expenditures could on average reach 1.5% of the GDP of MENA countries by 2015. Economic losses would result from rising mortality and morbidity, which would reduce labor productivity, capital investments, and shrink the labor force. HIV/AIDS surveillance systems to track the epidemic are particularly weak in the region. The lack of data combined with high levels of stigma and discrimination against high-risk groups and HIV-infected persons provide an optimal context for the disease to continue to spread silently.
The threat of HPAI pandemic is also very real for the region with bird cases already detected in Djibouti, Egypt, Iran, Iraq, Jordan, Kuwait, Saudi Arabia, and WBG and human cases confirmed in Djibouti, Egypt, and Iraq. Being centrally situated, the MENA region is geographically an important link between the origins of the infection in Asia and the rest of the world, not only in terms of migration of people but also of wild birds. By December 2007, Egypt had recorded 38 human cases of which 15 had died (a high 39% case fatality rate), the highest number of cases and deaths outside the East Asia and Pacific Region. While HPAI is still primarily a bird disease, there exists a significant risk to humans in close contact with infected birds, as is the case in Egypt.
Organization Of Health Systems
Both biomedical and traditional medical systems exist in the region and while the former predominates, the latter also provides a significant but difficult-to-quantify amount of services. The following subsections discuss the organization of both systems in MENA.
Organizational Structure Of Biomedical Health Systems
MENA health systems had traditionally been organized on the basis of the primary health-care (PHC) approach as a means of achieving the WHO-supported Health for All goals by the year 2000, but have gradually become more curative in focus. The goals called for health systems organized around the essential elements of PHC and this approach has contributed to improved health outcomes in the past. The current curative and hospital-based approach can neither effectively nor efficiently address the ongoing transitions. WHO assesses that MENA will have to address a number of identified weak areas including limited intersectoral cooperation; poor community involvement in planning and provision; weak policy analysis, formulation, coordination, and regulation; weak health information systems; poor organization and management of health services at all levels; and inappropriate human resource policies.
The provision of health services in MENA had primarily been the role of the state, with a centralized financing and delivery structure. More recently, with the governments’ inability to fully respond to the population’s health service needs, the private medical sector has been expanding to fill the gap in coverage with obvious equity, efficiency, and quality assurance concerns resulting from inadequate regulation by the governments. The private sector is now playing a dominant role in the health sector of MENA countries (with the exception of Gulf countries) and given their curative focus, they predominantly provide hospital-oriented and capital-intensive services requiring increased importation of drugs and medical technology.
By the income groupings already described, low-income countries have developed two-tiered health systems characterized by government and privately provided services. Although government services are subsidized and should be available to all citizens, in reality the quality is often suboptimal with inexperienced staff and poor availability of medical supplies and drugs. In addition, public services on the one hand do not fully cover rural and remote areas of these countries particularly in Yemen where there are significant physical barriers to rural populations accessing these services. Access to privately provided services, on the other hand, requires households to make direct out-of-pocket payments that can be impoverishing for the poor. As an example, in 2003, 95.5% of private health expenditures were out-of-pocket and public health expenditure accounted for only 40.9% of total health expenditures in Yemen (Table 3).
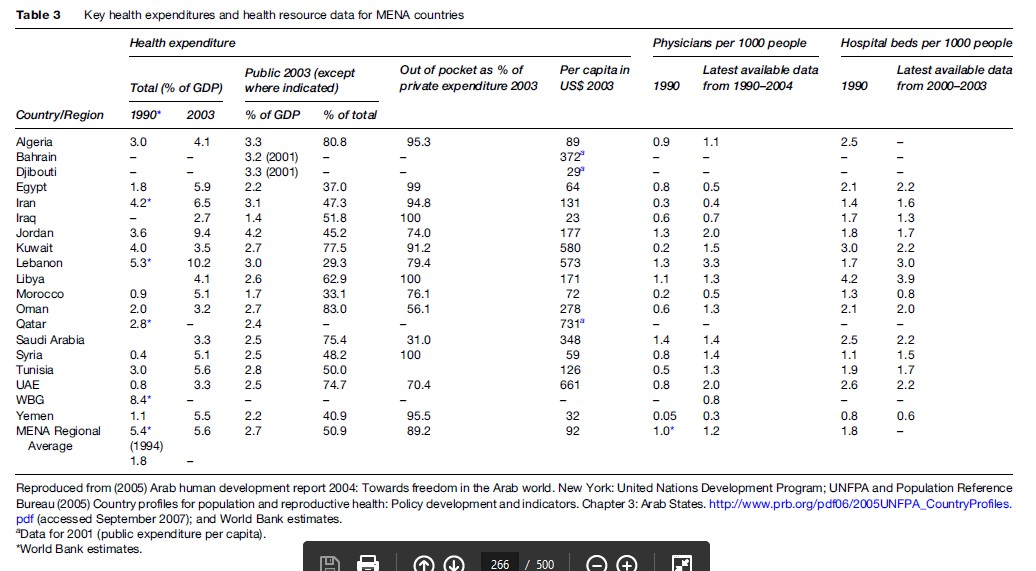
In middle-income countries of the region, governments have implemented reforms focusing on the financing and organizational aspects of health systems. Social health insurance systems have been implemented to varying degrees among these countries with many facing issues of population and service coverage particularly for workers in the informal sectors. The gaps in coverage have created the need for various providers including the private (for-profit and nonprofit) sector and the voluntary sector leading to fragmented health-care delivery and financing systems for these MENA countries. A number of these countries currently have to deal with rising health-care costs and inadequate financial protection at the consumer level. The Jordanian and Lebanese health systems are good examples with 9.4% and 10.2% of their respective GDP in 2003 spent on total health expenditures of which 45.2% and 29.3%, respectively, are the public expenditures. Out-of-pocket expenditures accounted for 74.4% ( Jordan) and 79.4% (Lebanon) of private expenditures on health (see Table 3).
With significant oil revenues, the upper-income countries have been able to achieve comprehensive health coverage for its population either free of charge or at highly subsidized rates. Evidence suggests however that this universal access, although generally affordable, could benefit from improved efficiency and quality reforms. Although per capita health expenditures are higher among these countries (ranging in 2003 from US $278 in Oman and US $731 in Qatar), more recently the GCC governments have had to implement cost-containment measures. They also face the challenge of providing health service coverage to foreign workers and their dependants.
Traditional Medicine Systems
The system of traditional medicine (TM) in MENA has a long history and is still available and used. The WHO terminology of TM is used here and is a comprehensive terminology that includes both TM systems (originating from the more long-standing settings of China and India) as well as other forms of indigenous medicine. TM in MENA has and is still largely based on an ancient system that is an amalgamation of the TM systems of China, Egypt, India, Iraq, Persia, and Syria and is referred to as Unani or Arab medicine. Unani, according to WHO, is increasingly being used in the region despite the more readily available modern medicine. The practice of this system however varies among countries depending on how it has been affected by the culture and history of each particular country. The history of religion is a significant influence and while the Islamic religion predominates, other religions such as Christian, Byzantine, Persian, Egyptian, Indian, Jewish, Mesopotamian, and Phoenician have also variously influenced TM in individual countries and subregions.
TM can generally be administered as medications or nonmedications with the former mainly including herbal medicines and the latter comprising various techniques which can be performed with or without medications. Common techniques include acupuncture, chiropractic, osteopathy, manual therapies, and other physical, mental, and spiritual mind and body therapies. Herbal medicine is the most common form of TM in MENA and the use seems to be increasing. For example, WHO/EMRO indicates that in UAE, there was a 3.85-fold increase in the importation of herbal medicine in 2001 as compared to 2000.
Nonmedication techniques available in MENA are diverse. In UAE, which has one of the most formalized TM systems in the region, nonmedication techniques include acupuncture, chiropractic, reflexology, osteopathy, and spiritual healing (mainly based on the Koran) and in Iran include bone-setting, massage therapy, and leech therapy.
Traditional birth attendants (TBA) are also an important part of the TM system in the region. They are patronized mainly by populations in remote and rural areas of most MENA countries where, in addition to age-long cultural practice of TBA, there are also significant physical barriers to accessing biomedical services. Surveys carried out by Khattab et al. (2000) in Saudi Arabia indicate that 38% of women in remote areas, despite high investments in the biomedical health systems by the Saudi Arabian government, preferred to patronize TBA, signifying their important role in the provision of maternal and child health services in the country.
In an environment in which the licensing of practitioners is generally absent or not well monitored, it is difficult to quantify clients that patronize TM practitioners. In many MENA countries, practitioners provide services that are not regulated and with the most poor in the population, mainly patronizing them due to easier physical and financial access. It should be noted, however, that even the more wealthy and educated populations in the region simultaneously use the services of both traditional and biomedical health systems.
Globally, WHO classifies four main types of national policies on TM: integrative, inclusive, tolerant, and exclusive. Few countries globally adopt the two extremes of integrated (four countries) and exclusive (even fewer) TM policies. These policies are important to define the role of TM in national health-care systems, allowing for regulatory and legal mechanisms to ensure good practice. While TM is generally accessible and affordable in many MENA countries, it is insufficiently integrated into national health systems and policies to guide its regulation and thus use does not occur frequently.
In 2000, WHO/EMRO carried out a survey on the regulation of herbal medicines in 22 MENA countries. Thirteen countries responded, of which five have national policies on TM as a whole, eight have herbal medicine regulation, nine allow herbal medicines to be legally sold without registration, and five have national institutes of herbal medicine. Kuwait is the first country (in 1984) in the region to have its constitution recognize Islamic TM and have a herbal medicine regulation separate from the regulation of conventional medicine. An Islamic medical center established in 1985 tests the safety of commonly used herbal medicines before they are then produced in the center’s laboratory. The center works together with medical doctors, scientists, and traditional practitioners and it is not uncommon for doctors to diagnose patients and the traditional practitioners to prescribe the treatment, which is covered by government health insurance schemes.
In 1996, UAE established a research center for herbal and traditional therapy exclusively. The center works together with the Ministry of Health (MOH) to regulate and register herbal products. Iran has a long history of TM and is very rich in medicinal plant resources (estimated at more than 8000 medicinal plants). The government has been supporting the development of a national inventory of its medicinal plants of which at least 2500 have been listed and classified. The country has TM research and educational facilities in seven out of its 30 provinces. A national academy of TM was established in 1991 in the country with the objectives of supporting herbal medicine research, studying the history and trying to maintain TM, conducting educational research and recommending educational plans on TM to the MOH, and educating the public on the rational use of TM. A panel of experts established by the government had facilitated the inclusion of herbal medicines on the list of essential drugs and the registration of locally produced herbal medicines. By the end of 2004, there were more than 300 licensed herbal products in the country. Jordan and member states of the GCC have also more recently started the process of developing guidelines for the regulation of herbal medicine.
WHO/EMRO has implemented TM strategy (2002–05), with the following four key objectives:
- To integrate relevant TM with national health-care systems by developing and implementing national TM policies;
- To promote safety, efficacy, and quality by expanding the TM safety, efficacy, and quality knowledge base, and by providing guidance on regulatory and quality standards;
- To increase the availability and affordability of TM;
and
- To promote the rational use of TM by providers and consumers.
The organization has also been supporting countries’ efforts at developing national guidelines and policies and is planning to publish regional guidelines in 2007.
Human Resources Issues In MENA Health Systems
The human resource situation in the region, an important input for quality health-care services, varies among and within countries in terms of quality, quantity, and distribution. MENA health systems also face the same global challenges of training, sustaining, and retaining health personnel. Table 3 includes the number of physicians per 1000 population in 1990 and in 2004. The average for the region in 2004 was 1.2 per 1000 population, which is lower than would be expected for a region largely composed of middle and high-income countries. Yemen, Morocco, WBG, Iran, and Iraq have the lowest number of physicians while Lebanon, Jordan, and UAE have the highest number per 1000 population. The quantity of other allied medical staff follows the same general trends as for physicians.
Similar to international trends, most health staff in the region are concentrated in urban areas. Rural areas, despite having the physical health infrastructure, usually lack adequate staffing not only in terms of numbers but also in terms of the required gender and experience of available staff. Access to services by patients in rural areas is therefore limited in terms of general unavailability of staff (including the limited and inconvenient hours those that are actually present work) and of qualified staff to address specific needs. There is also a shortage of female staff, which is a significant barrier given that for cultural reasons women and girls require female staff to provide their services.
There are also insufficient numbers of public health practitioners to address the ongoing epidemiological transitions in the region. Rawaf (2004) notes that public health practitioners – especially physicians – have a low status and low incomes and this factor, along with underdeveloped public health capabilities and infrastructures, lack of structured training and career development opportunities, and lack of data are a significant human resource challenge for the region. Appropriate policies and management of human resource issues are essential for integrating preventative and health promotion services with curative services and should also be factored into strengthening the curricula of training institutions in the region.
Pharmaceuticals And Medical Equipment And Technology
According to WHO/EMRO less than half of MENA countries have adopted or are actively implementing national drug policies and yet less than a third of the population has regular access to essential drugs. In the absence of functional pharmaceutical regulations, irrational drug prescribing and self-medication are still major challenges in the region despite the availability of essential drug lists and an abundance of treatment guidelines. The availability of prescription medications in private pharmacies makes self-medication relatively easy. The use of brand name medications instead of generics is also relatively common and this together with the irrational prescription habits contributes to the high proportion of total health spending on pharmaceuticals in the region. Developing more effective and better-regulated national procurement arrangements can also reduce pharmaceutical spending in countries.
Spending on medical equipment and technology in MENA is also very significant and inefficient. Given the highly curative, specialized, and hospital-based model in both public and private sectors, this should not be surprising. With the large surpluses of hospital beds and physicians, the spending on this category of expenditure can be significantly rationalized for efficiency goals.
National Health Accounts
MENA countries can sufficiently track their health expenditures by broad categories of public versus private sources of funding (see Table 3) and, to some extent, expenditures on different health inputs such as staffing, drugs, technology, medical supplies, administration, and so on. By international standards, however, MENA countries generally lag behind in their ability to develop and implement national health accounting (NHA) systems that are comprehensively and methodologically consistent. In the absence of comprehensive NHA, tracking of health expenditures and resource allocation for cross-country comparisons and more importantly for communicating relevant policy-making information to key stakeholders/decision makers is extremely difficult. In particular, public health policy makers and practitioners in the region lack the comprehensive information they require to determine additional financing needed for public health and which services should be chosen for priority funding and by source of funds.
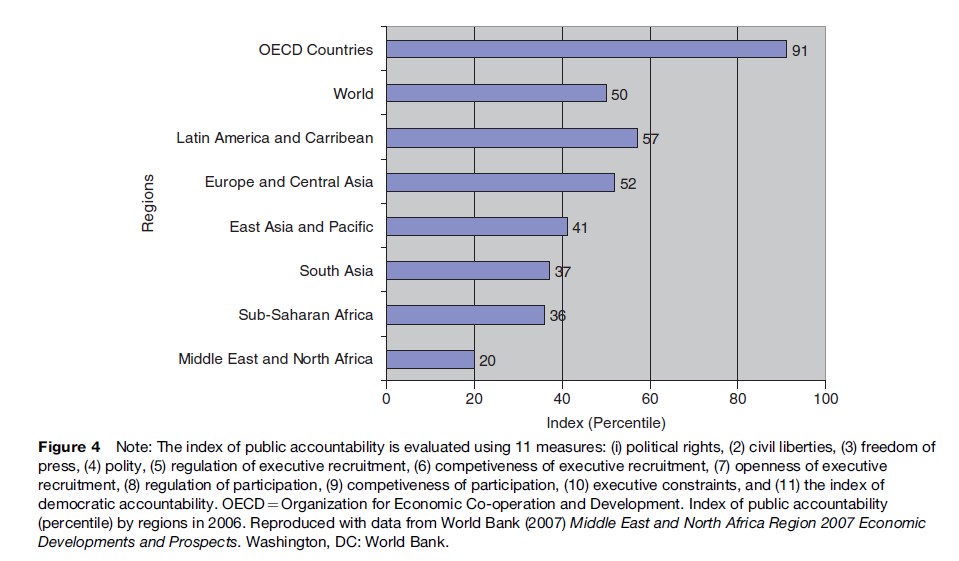
Governance And Its Effects On MENA Health Systems
Governance refers to a set of rules and the processes governing the exercise of authority in the name of a constituency; good public governance entails inclusiveness and accountability. The effectiveness of a health system will depend on the extent to which those who deliver the services are held accountable for their performance. The weak performance by MENA governments is linked to weak governance mechanisms and some deficiencies in health service delivery can be attributed to the weak public and social accountability. As noted by the 2004 Arab Human Development Report, participation in government by civil society is weak; no questions are asked of governments, nor are they held accountable for their performance. The MENA region lags behind others in terms of participatory governance (Middle East Quarterly, 2002) and has the lowest index of public accountability among all regions of the world according to World Bank data that use this index along with others to evaluate governance quality (Figure 4). Effective and efficient health systems require partnerships between the health and non-health sectors as well as between government and a variety of other stakeholders including the private sector, nongovernmental organizations, and households and individuals. The existing governance structures limit the interaction between governments and other key stakeholders leading to centrally managed health systems. Many MENA governments are now exploring more pluralistic methods for managing their health systems but this will require a governance structure that includes clearly defined institutional roles for different actors and a central government that not only provides better strategic direction for planning and policymaking but also better monitors and regulates policy implementation by the various stakeholders.
Challenges To MENA Health Systems
Health Transition-Related Challenges
MENA health systems are under increasing pressure to keep pace with epidemiological and demographic transitions. The growing population implies that the cost of providing health services will continue to increase because more people (refugees and foreign workers included) will require basic services, more females will require reproductive health services, more young people will require youth-friendly services, and the aging population will require specialized care. MENA health systems have to adapt to address all these transitions within an environment of limited resources. New approaches and paradigms are needed in the reorganization of the health-care delivery system, which should feature among others better partnerships by different stakeholders and providers; redistribution of skills mix and enhancing the knowledge of health professionals; and the rationalization of existing pharmaceuticals and medical technologies and the appropriate introduction of new ones.
With the current curative model of care focusing largely on acute care, MENA health systems could greatly benefit from a more strengthened primary health-care approach that not only provides regular and extended care to patients but one that integrates preventive and health promotion services together with curative services. Patients and their households have a central role to play in the management of chronic conditions since they require daily lifestyle and behavior changes. Health systems must be involved in empowering patients to play a more active role in own their care and to link patients to community services that can support their efforts.
The emergence of new diseases such as HIV/AIDS and HPAI has underscored the need for more effective surveillance systems as an important part of an overarching national monitoring and evaluation system needed to track not only these emerging infections but other existing conditions. A review of disease surveillance systems by WHO/EMRO notes that there is insufficient commitment to the systems, lack of practical guidelines, overwhelming reporting requirements, weak involvement of the private sector, lack of transparency, shortage of human resources, and poor data analysis. In the absence of efficient surveillance systems, it becomes difficult to effectively plan and implement measures that proactively curb the widespread transmission or the onset of diseases and to provide timely services for those who need them.
Health Systems-Related Challenges
Together with the adaptation of MENA systems to address health transition challenges is the need to concurrently address systemic ones related to issues of equity, efficiency, and sustainability. To address these challenges, political commitment, resources, and management capacity are needed to strengthen existing public health functions or develop them where they are absent. The most critical of these functions include intersectoral policy making, public information and education, and quality assurance. The management of these functions can only succeed where transparent governance structures exist and where more complex coordination among the different entities beyond the health sector can take place.
Equity considerations will require improving the various dimensions of access to health services but also an extension of financial protection to those who most need it. With the exception of a few countries (Saudi Arabia, Oman, and UAE) out-of-pocket expenditures accounted for at least 74% of private health expenditures in 2003 (see Table 2), which disproportionately affects the poorer populations who can be further impoverished in the event of a catastrophic illness. MENA governments are increasingly interested in extending financial protection and improving access to health services by using different risk-pooling mechanisms, including social and private health insurance and could benefit from global experiences at achieving these. Well-targeted social safety nets are needed to ensure adequate protection of citizens against the impoverishing effects of ill health.
Addressing the efficiency concerns will require a shift from the current curative care model together with more comprehensive rationalization of health resources. In general there are more hospital beds than needed in most countries of the region and particularly in the public sector, which have a regional average of 80% of the beds but less than 65% occupancy rates. Maintaining this excess capacity has resource implications. Instead of the current focus on expanding the hospital-based infrastructure, more critical is the need to reconfigure the MENA health system to better integrate the provision of preventative and promotion services with treatment and support services. With the growing population, MENA health systems require a stronger emphasis on services and functions aimed at reducing the population’s level of exposure to existing risks of emerging challenges rather than the more expensive option of treating them when affected.
Improving and sustaining achievements of national health systems in the region becomes even more challenging within the context of a growing population and especially one with a high economic dependency rate. With 58% of the population less than 25 years of age and the highest unemployment rate, the proportion of the MENA population that is economically active is the lowest in the world. This has implications on how health insurance schemes in the region (social and private) can be more efficiently managed and maintained. The high dependency ratio adds more fiscal pressure on limited government health budgets, which need to be better targeted at addressing the needs of the most vulnerable populations. Governments can also take better advantage of the growing private health sector by fully regulating them and ensuring that private along with public investments are invested in more cost-effective technologies.
Addressing the systemic challenges will require a more comprehensive health information system that provides relevant data that are readily available for assessing priorities as well as for planning, managing, and implementing the required services. Unfortunately, the region generally lacks available, reliable, timely data to guide these processes. National and regional research and development capabilities will need to be strengthened to contribute to health information systems. Expenditures for research and development in the Arab world are still relatively low and yet there is a great need to develop local expertise in the collection, interpretation, presentation, and dissemination of data.
Conclusion
The region clearly faces a multitude of challenges at various levels and scope, with some easier to address than others. Governments have the complicated task of defining the priorities and determining the best options for addressing them within budget-constrained environments. This process will require a more thorough assessment of the situation than is currently available. Investing in this assessment will be money well spent provided it informs and supports the required changes to the systems to make them more responsive and efficient. To effectively and efficiently respond to these challenges, MENA governments must also have the political will to involve key stakeholders in the planning, implementation, and management of health systems.
The MENA region is not alone in trying to keep pace with the current and future health-related transitions because all other regions also have their own similar and yet unique sets of challenges. The beauty of globalization is that regions and countries can benefit from others and share their experiences in tackling these challenges.
Bibliography:
